An Introduction to Conventional Aligner Biomechanics
Clear aligner therapy utilizes a series of custom-made tooth ‘aligners’ to gradually straighten teeth and align the bite. Each aligner in the series is formed with small incremental movements incorporated which cause the aligners to deflect and stretch over the teeth when they are inserted. As the aligners attempt to spring back to their original shape, force is delivered to the teeth thereby producing tooth movement. The greater the deflection, the larger the activation force produced by the aligners.
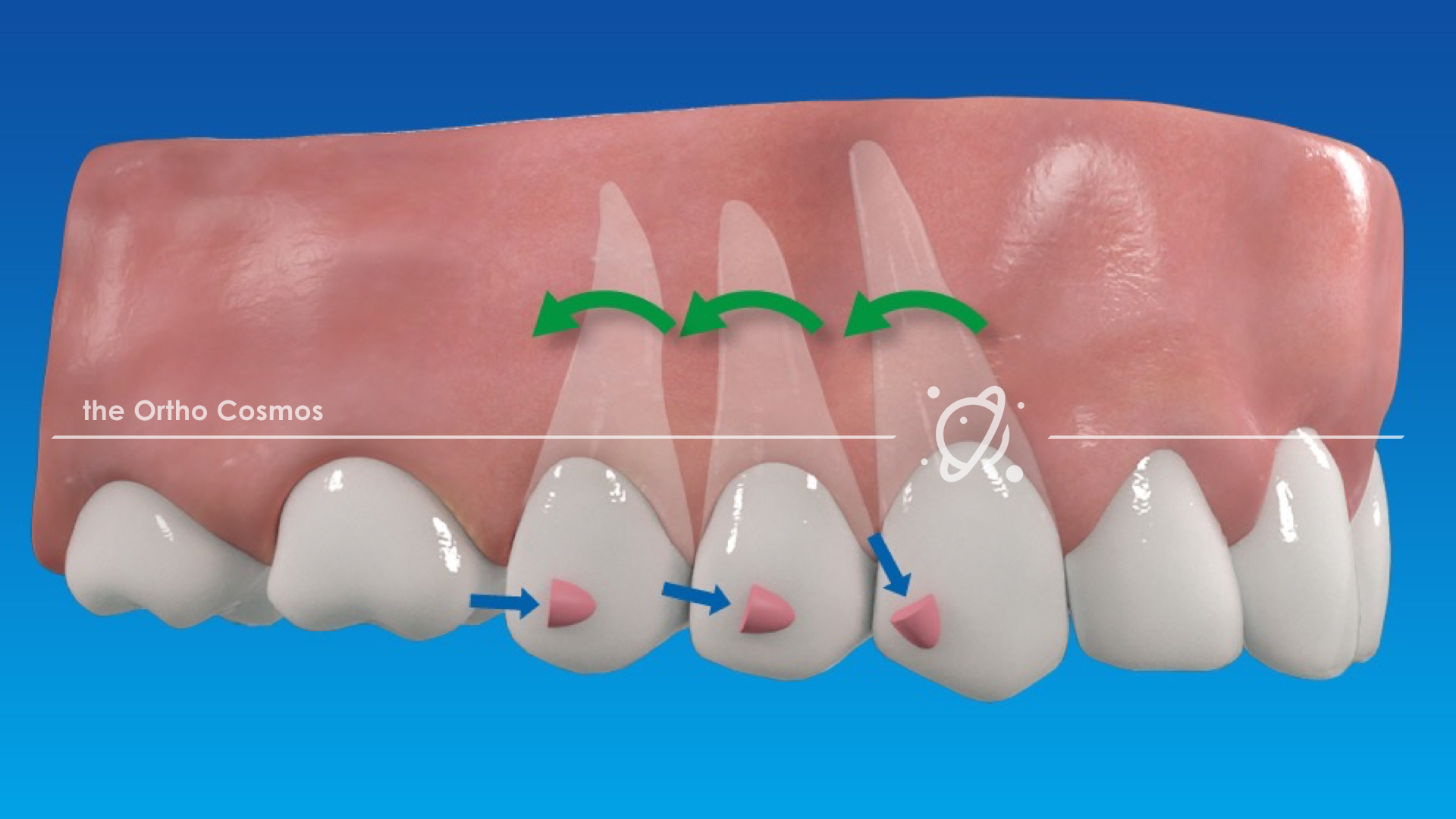
Early on in the development of this treatment modality, it became evident that certain types of tooth movements would response unpredictably due to the way teeth are shaped, like trying to pick up a wet watermelon seed. The logical solution to this dilemma was to allow clinicians to alter the shape of the teeth by bonding ‘attachments’ to provide control over where and how forces are delivered. Thus conventional clear aligner biomechanics were born.
The ‘Conventional’ approach is based on three central premises:
- Attachments serve as the primary interface for force delivery and the active surface area(s) of attachments must be oriented to maximize the attachment/aligner interaction in relation to the vector of force applied to the tooth. These active “pushing” surfaces must also be positioned as perpendicular as possible to the vector of force being applied.
- The active pushing surfaces of attachments can be positioned to provide proper force systems without any additional thermoforming modifications to the aligners.
- A visual assessment of force vectors by the clinician is sufficient for the designing effective force systems using attachments
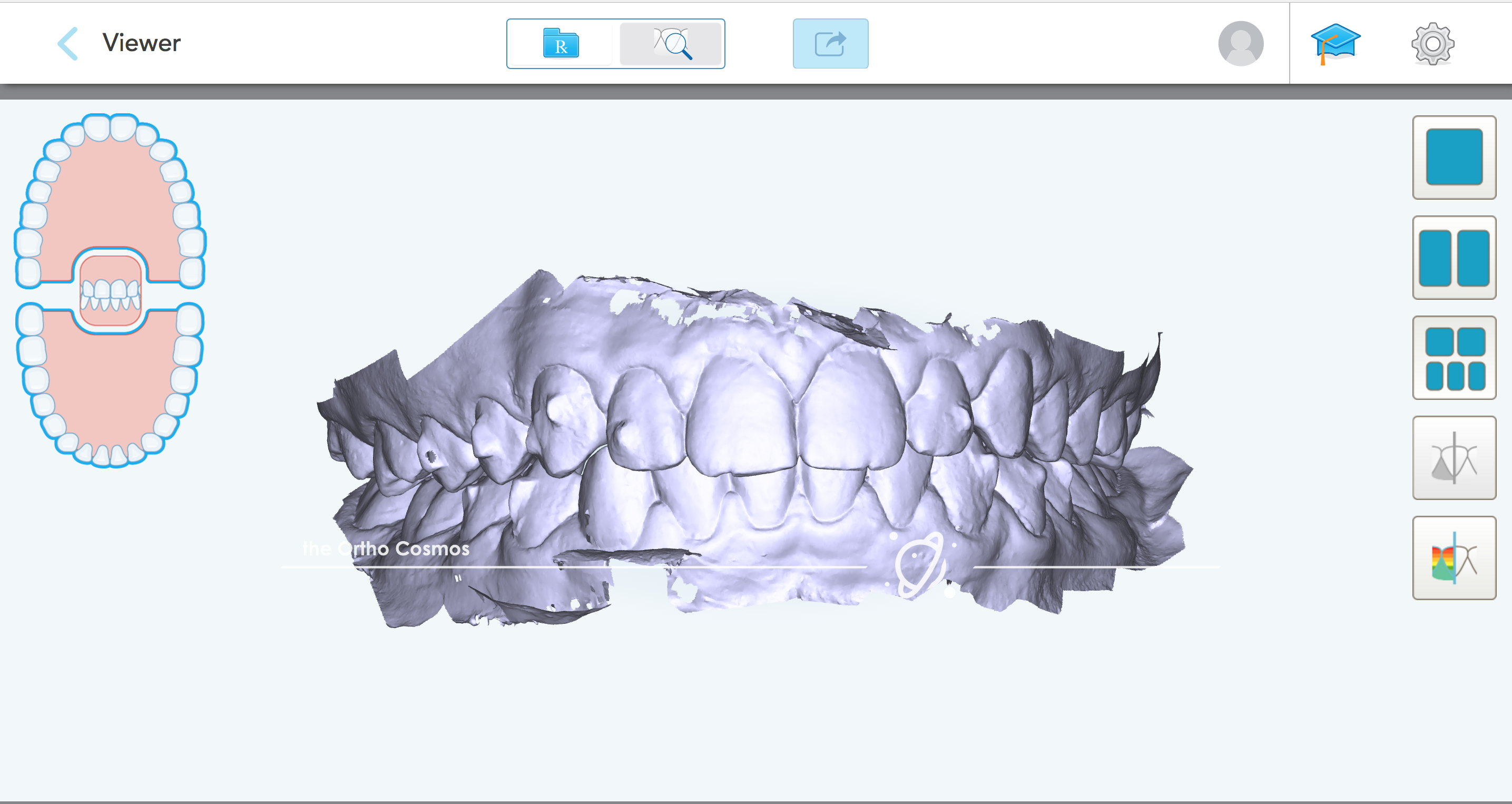
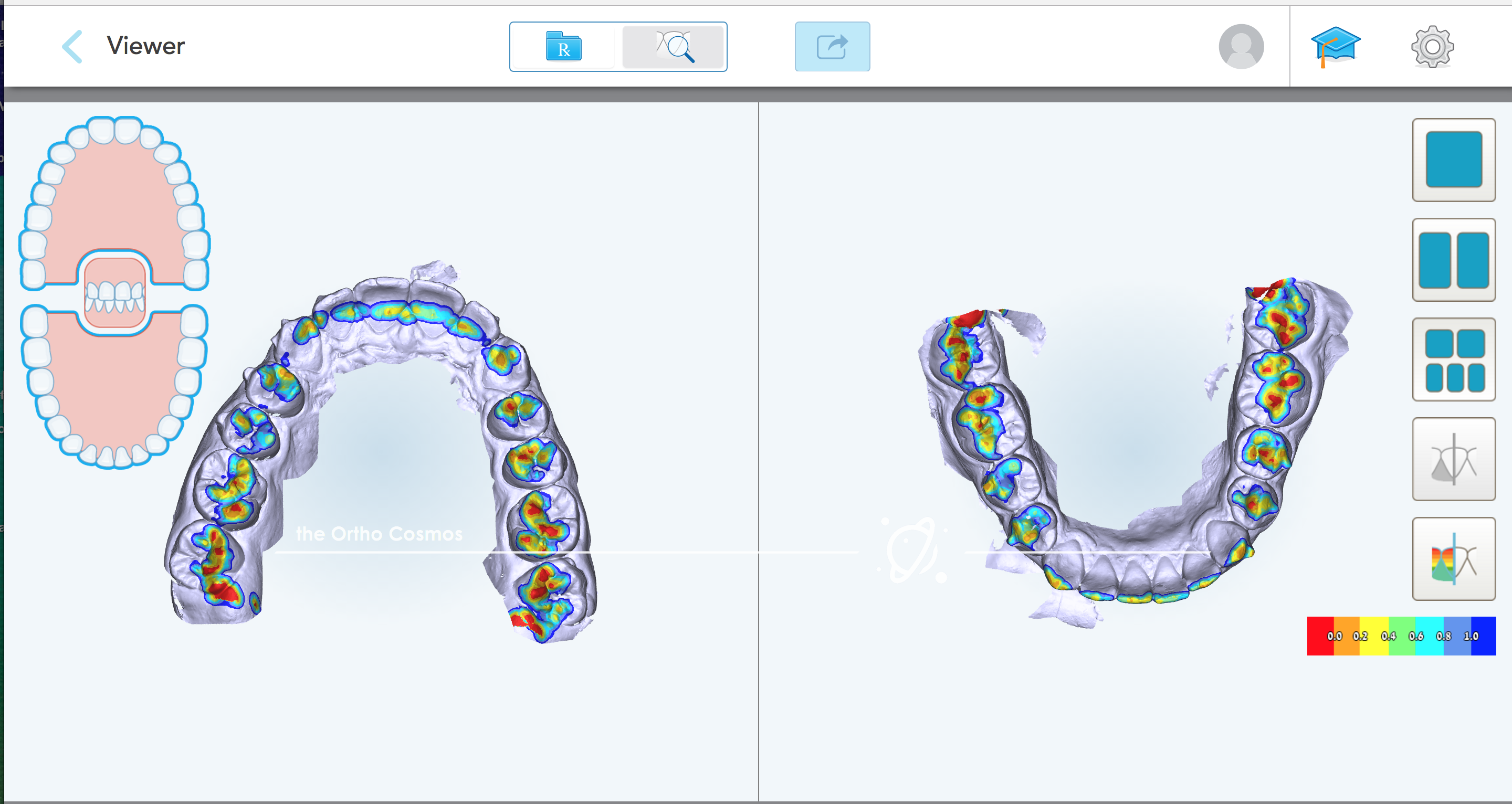
Although this philosophy has been employed in clinical practice for many years, the conventional wisdom behind these mechanics has received limited scrutiny. Both Sean Holliday and myself sought to help remedy gaps the specialty’s understanding of clear aligner mechanics by creating digital simulations of various tooth movements using CAD software. Through this approach we were able to evaluate the efficacy of various attachment designs by visualizing and comparing the prescribed initial force systems with a heat map.
We tested many iterations of attachment designs and movement combinations to determine which designs were most desirable for different clinical situations. While there isn’t time to wade through the entire exhaustive library of possible permutations here in this post, the initial force heat-maps for mesial root tip with just a few of the attachment designs we evaluated should help to reveal the clinical realities of clear aligner biomechanics. We also begin to see that the underlying assumptions of conventional, attachment-driven, clear aligner mechanics outlined above are fundamentally flawed.
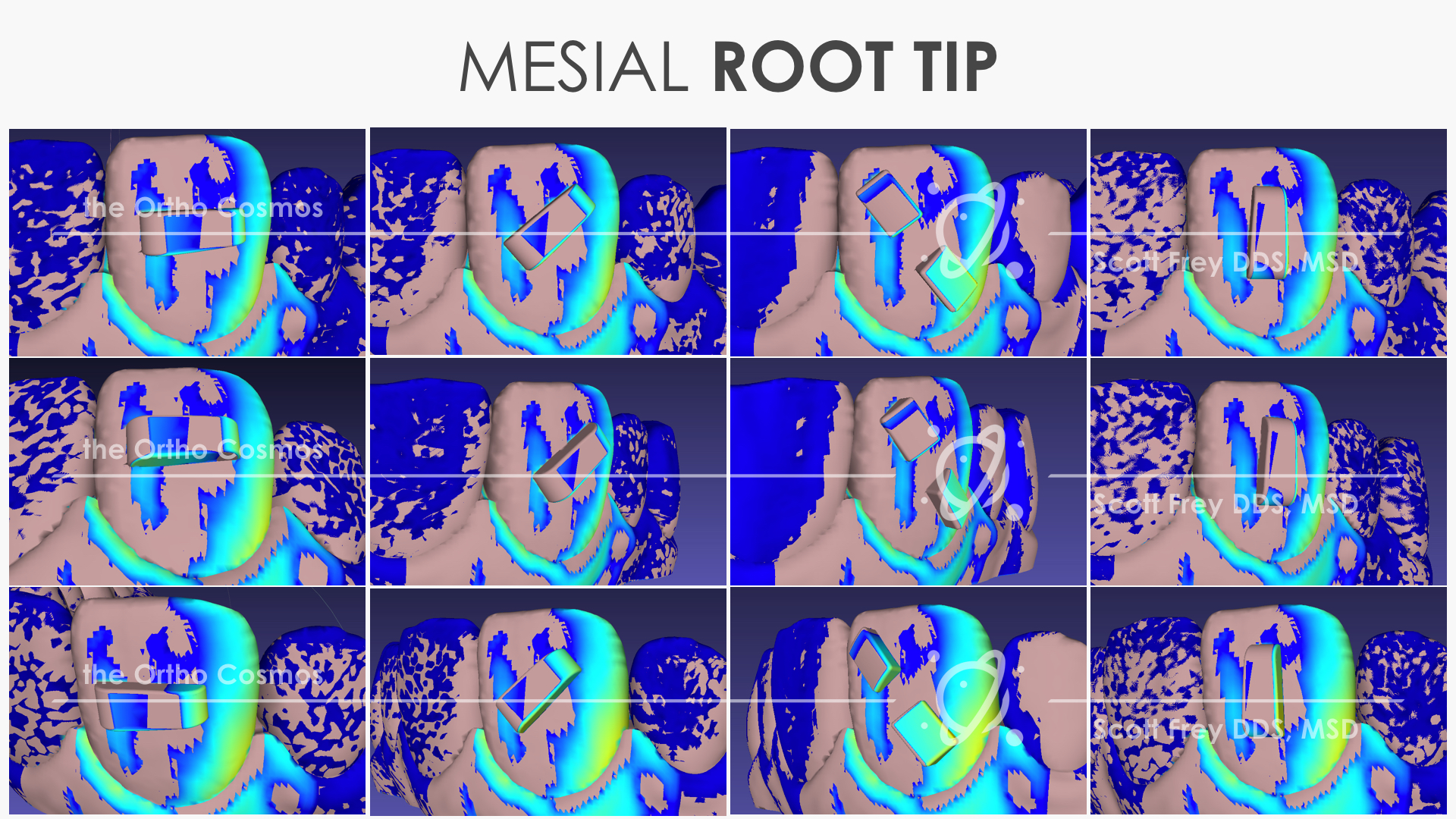
In the heat maps above it is apparent that the attachments alone will fail to provide clinicians with precise or sufficient levels of root control. In many cases, the moment-of-force and moment-of-couple are not provided by the attachment at all, and when the moment-of-couple does exist on the attachment itself numerous interferences exist which will degrade the intended force system.
We can draw the following conclusions regarding clear aligner biomechanics:
- Visual assessment of force systems is not effective. We know it does not work for fixed appliances and this proves doubly true for clear aligners because we are unable to adequately anticipate interferences and/or unseating of the aligners that will occur during activation and over the course of treatment. Without accounting for these factors the aligners will not be able to consistently deliver the intended force systems.
- Customized thermoforming features are an essential part of establishing proper force systems with clear aligners. Attachments frequently serve only a supporting role in force delivery by helping to achieve more complete seating of the primary thermoforming features. Additionally, key attachment surfaces can be rendered insert by certain movement combinations without specific thermoforming features being incorporated in the aligner.
- Attachment-driven mechanics require significant lag and/or overcorrections of tooth movements in order for the aligners to engage attachment surfaces in the manner intended for root control. This decreases the predictability of force systems, results in excessive staging and slower treatment, and thus increases manufacturing demands because more aligners must be produced. Increase attachment size and alter orientation to enhance active attachment surface area in the relation to the vector of force
These findings run counter to the existing clear aligner dogma across the specialty, but they are consistent with the numerous proprietary features that Invisalign has incorporated into their clear aligner system following extensive internal data mining. Going forward with this knowledge, we have several recommendations for clinicians to help them improve their success with clear aligner therapy:
- Clinicians must consider aligner forming features as the primary force interfaces instead of attachments. Thus, attachments that are used can be made smaller and can be applied far less frequently than conventional wisdom suggests.
- A means of adding and modifying thermoforming features (both for relief and activation) must be a focus of the continued development of clear aligner systems in order to provide clinicians with better force systems for root control during treatment. Currently, Invisalign is the only clear aligner system that has incorporated customized thermoforming features and many are proprietary.
- Clear aligner companies and clinicians must leverage extensive clinical data artificial intelligence for efficient clear aligner therapy. Data-mining is essential to clinical application of clear aligners and necessary to augment our own clinical skill sets.